Menstruation is a natural biological process that signifies the shedding of the uterine lining in the absence of pregnancy. While the experience of menstruation varies widely among individuals, the occurrence of blood clots during periods is a common phenomenon that can raise questions and concerns.
These clots, typically a mixture of blood cells, tissue fragments, and proteins that help regulate bleeding, are usually harmless and a normal part of the menstrual process. The presence of unusually large or numerous clots can sometimes indicate underlying health issues that require attention.
Knowing the top causes of blood clots during periods is crucial for recognizing when menstrual patterns may be normal or when they might signify a need for medical consultation.
Key Takeaways:
- The commonest causes of blood clots are natural menstrual cycle processes, hormonal imbalances, uterine fibroids, endometriosis, adenomyosis, and blood coagulation disorders.
- Blood clots are a common part of menstruation, consisting of blood cells, uterine tissue, and proteins.
- Imbalances in estrogen and progesterone can cause menstrual irregularities, including changes in bleeding volume and clotting.
1. Natural Menstrual Cycle Processes
During a menstrual cycle, the body naturally prepares for a potential pregnancy by thickening the lining of the uterus. If pregnancy does not occur, this lining—comprised of blood, tissue, and nutrients—is shed, leading to menstruation. Blood clots during periods are a natural phenomenon, primarily due to this shedding process. They are a mixture, and consist of:
- Blood cells
- Tissue from the lining of the uterus (endometrium)
- Proteins in the blood that assist in regulating bleeding
Blood flow rate plays a crucial role in clot formation. Normally, the body produces anticoagulants to prevent menstrual blood from clotting as it is being shed. However, during periods of heavy flow, these anticoagulants may not work quickly enough, allowing clots to form.
This is often why clots are more common and larger during the heaviest days of menstruation. The consistency and amount of menstrual blood can vary significantly from person to person and can even change at different stages of an individual’s life.
While small clots are generally not a concern, unusually large or numerous clots can indicate underlying health issues. Understanding these natural processes is crucial for distinguishing between normal menstrual variations and potential health concerns that may require medical attention.
2. Hormonal Imbalances
Hormonal imbalances, particularly involving estrogen and progesterone, can significantly impact menstrual health. These hormones play key roles in regulating the menstrual cycle, including the preparation of the uterine lining for pregnancy and its subsequent shedding if pregnancy does not occur.
When these hormones are out of balance, it can lead to various menstrual irregularities, including heavier or lighter periods, irregular cycles, and increased blood clotting. For instance, high levels of estrogen can cause the uterine lining to thicken more than usual, leading to heavier menstrual bleeding and potentially more significant clotting when the lining is shed.
Conversely, low levels of progesterone may not adequately support the uterine lining, causing it to shed irregularly and possibly increasing clot formation. Thyroid disorders, such as hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid), can also affect menstrual bleeding.
The thyroid gland plays a crucial role in regulating the body’s metabolism, which includes influencing menstrual cycles. An imbalance in thyroid hormones can lead to changes in menstrual patterns, including the amount of bleeding and the presence of clots.
3. Uterine Fibroids

Uterine fibroids are non-cancerous growths that develop in or on the uterus. Several factors can determine their development:
- Size
- Location
- Number
Fibroids can cause a range of menstrual irregularities, including heavy menstrual bleeding (menorrhagia) and significant clotting. Submucosal fibroids, which grow in the inner layer of the uterus, and intramural fibroids, which grow within the muscular wall of the uterus, are particularly likely to cause heavy bleeding and clotting.
These fibroids can lead to heavier and more prolonged periods as they increase the surface area of the endometrium that needs to be shed and can disrupt normal uterine contractions that help control menstrual flow.
The increased bleeding can overwhelm the body’s ability to produce anticoagulants, resulting in the formation of clots. While the exact cause of fibroids is not fully understood, hormonal factors, particularly estrogen and progesterone, appear to play a significant role in their growth.
Treatments for fibroids that cause heavy bleeding and clotting can vary, ranging from medication to manage symptoms to surgical options for removing fibroids or, in severe cases, the uterus itself.
4. Endometriosis
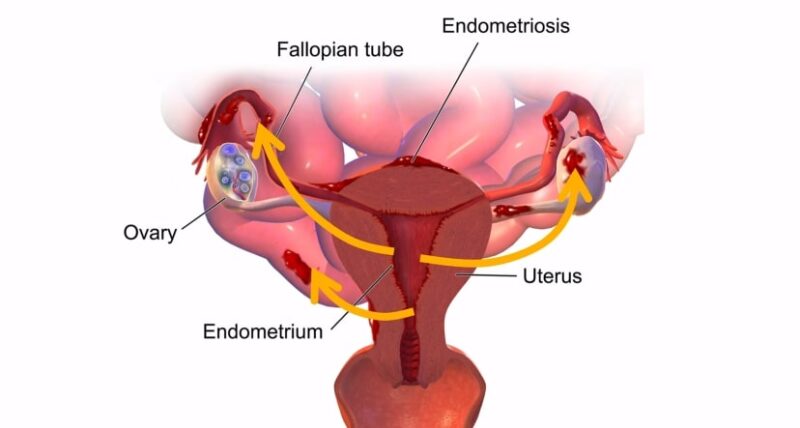
Endometriosis is a condition where tissue similar to the lining of the uterus begins to grow outside the uterine cavity, such as:
- On the ovaries
- Fallopian tubes
- Other pelvic organs
This endometrial-like tissue behaves in the same way as the tissue lining the uterus—it thickens, breaks down, and bleeds with each menstrual cycle. The blood and tissue shed from endometrial growths have no way to exit the body, leading to pain, inflammation, and the formation of scar tissue and adhesions.
This condition can cause significantly heavier menstrual bleeding than normal, as well as the presence of larger or more numerous blood clots. The increased volume of blood and tissue being shed both from the uterus and the abnormal endometrial growths contributes to the formation of clots during menstruation.
The pain associated with endometriosis, particularly during periods, can be severe and debilitating. It often correlates with the extent of the condition but is not always indicative of the severity of the disease. Treatment for endometriosis may include pain management, hormone therapy to reduce or eliminate menstruation, and surgical options to remove endometrial growths or the uterus in severe cases.
5. Adenomyosis
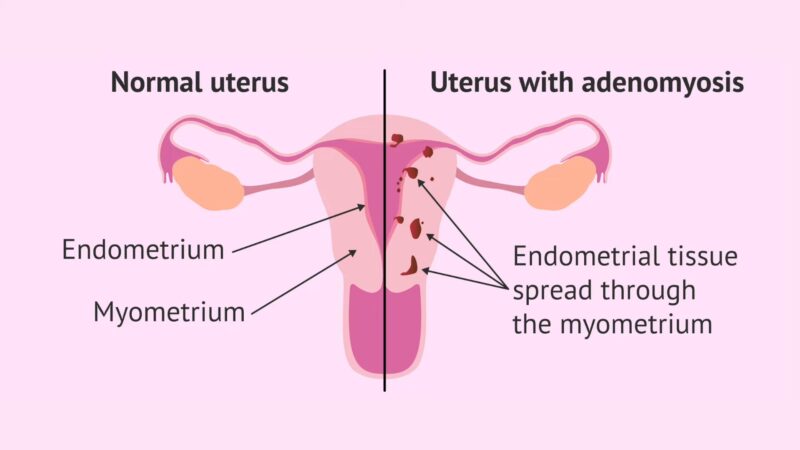
Adenomyosis occurs when the endometrial tissue, which normally lines the uterus, begins to grow into the muscular walls of the uterus. This condition can lead to a thickened uterine wall, heavy and painful periods, and the presence of large blood clots.
Unlike endometriosis, where the tissue grows outside the uterus, adenomyosis affects the uterus internally, causing the endometrial tissue to break down within the muscle wall during menstruation. This internal bleeding within the uterine muscle can lead to increased menstrual flow and the formation of blood clots.
The pain associated with adenomyosis is often described as intense and may be accompanied by pressure and bloating in the lower abdomen. The cause of adenomyosis is not entirely understood, but its development has been linked to hormonal factors and uterine inflammation.
Treatment options for adenomyosis aim to alleviate symptoms and may include anti-inflammatory medications, hormonal treatments to control menstrual bleeding, and, in severe cases, surgical procedures such as hysterectomy. Managing adenomyosis and its symptoms requires a comprehensive approach that considers the severity of the condition, the patient’s symptoms, and their reproductive plans.
6. Blood Coagulation Disorders
Blood coagulation disorders can significantly impact menstrual bleeding, leading to heavier periods and the formation of blood clots. These disorders affect the blood’s ability to clot properly, which can result in excessive bleeding during menstruation.
Von Willebrand Disease (VWD) is one such condition that can cause heavy menstrual bleeding due to a deficiency in or dysfunction of the von Willebrand factor, a protein that is crucial for blood clotting. Similarly, platelet function disorders can lead to abnormal bleeding and clotting during periods.
Platelets are small blood cells that play a key role in blood clotting, and any dysfunction in their activity can result in increased menstrual flow and clot formation.
FAQs
What do endometriosis clots look like?
Endometriosis clots can vary in appearance but often look similar to regular menstrual clots—dark red and jelly-like. They may appear larger or more abundant due to heavier menstrual bleeding associated with endometriosis.
What do fibroid blood clots look like?
Fibroid blood clots also resemble typical menstrual clots, being dark red and gelatinous in texture. The presence of fibroids may lead to heavier bleeding, resulting in larger or more frequent clots.
How big is too big for period clots?
Generally, period clots larger than a quarter in size may be considered too big and could indicate an underlying health issue. If you frequently pass clots this size or larger, it’s advisable to consult with a healthcare provider.
What color is fibroid period blood?
Fibroid period blood can range from bright red to a darker maroon color. The bleeding may be heavier and more prolonged, potentially altering the color and consistency of the menstrual blood throughout the period.
The Bottom Line
The formation of blood clots during menstruation is a complex interplay of natural bodily processes, hormonal balances, and potential underlying health conditions.
While the presence of small, occasional clots is typically not a cause for concern, significant changes in menstrual bleeding patterns, such as the appearance of large or numerous clots, warrant medical attention.
Conditions like hormonal imbalances, uterine fibroids, endometriosis, adenomyosis, and blood coagulation disorders can contribute to abnormal clotting and may require targeted treatments to manage symptoms and underlying causes effectively.
